Picture this: You’ve always had regular periods, but lately, things feel different. Maybe you’re experiencing unexpected mood swings, or your sleep isn’t what it used to be. Perhaps you’re having occasional hot flashes, but your periods are still coming – just not as predictably as before. You’re wondering: Is this perimenopause, or am I in menopause?
As a dual-certified physician in both Family Medicine and Functional Medicine, I hear this question almost daily in my practice. The confusion is completely understandable – but understanding the difference between these two phases is crucial for your well-being. Why? Because waiting to seek help until you’re officially in menopause means potentially suffering through years of manageable symptoms. The good news? Most symptoms can be effectively treated, and you don’t have to simply “tough it out.”
What is Perimenopause?
Perimenopause is the transitional phase leading up to menopause, and it often catches women by surprise. While the average age range is 45-55, I’ve treated many women who begin experiencing changes as early as 35. This transition can last anywhere from 2 to 10 years – yes, you read that correctly – and it’s different for every woman.
What Actually Happens During Perimenopause?
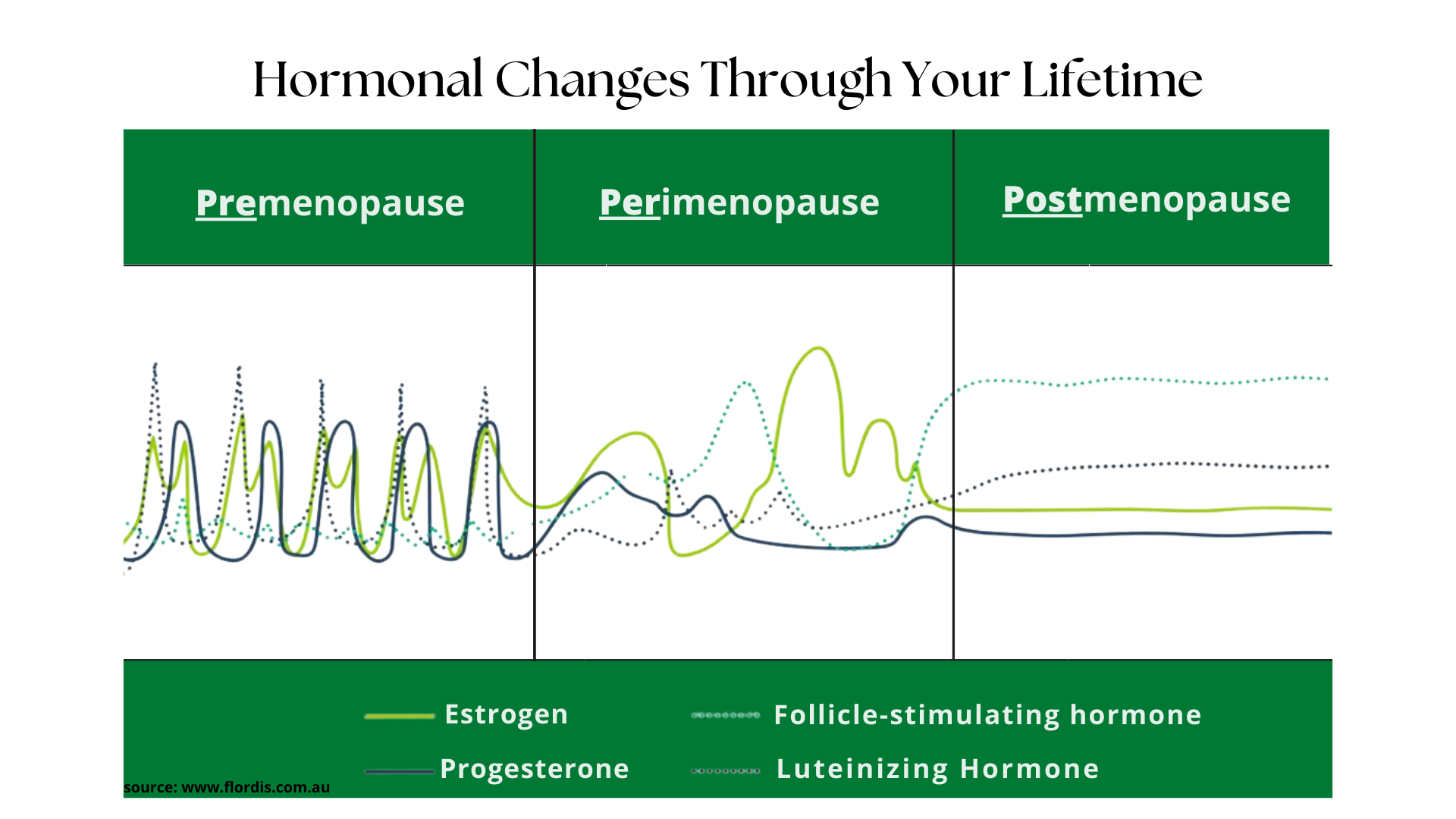
The key characteristic of perimenopause is irregularity. Many women miss these early signs because they’re subtle. For example, if your cycles were always 28 days, you might start having 25-day cycles one month and 31-day cycles the next. This is your body’s first whisper that hormonal changes are beginning.
Important note: You can still get pregnant during perimenopause. I’ve seen many surprised women in my practice who thought they were too old for contraception – don’t make this assumption!
Common Perimenopause Symptoms
During my years of practice, I’ve observed that perimenopause can include:
- Missed periods if you have had intercourse and do not have contraception (Get a pregnancy test!)
- Hot flashes and night sweats
- Mood fluctuations
- Disrupted sleep patterns
- Weight changes, particularly around the midsection
- Brain fog (those “where did I put my keys?” moments)
- Vaginal changes
- Decreased libido
What is Menopause?
Here’s where we get technical: Menopause is officially diagnosed after 12 consecutive months without a menstrual period. The average age is 51, but what’s “normal” spans a wide range. It’s important to understand that menopause can be natural or induced (through surgery or medical treatments). Interestingly, if menopause is induced but the ovaries are retained, you’ll likely still experience perimenopause symptoms.
The Hormone Story of Menopause
During menopause, your hormone levels become consistently low, unlike the roller coaster of perimenopause. This leads to permanent changes in your body, including:
- Complete end of menstruation
- Inability to conceive
- Continued hot flashes (though often less severe than in perimenopause)
- Changes in bone density
- Cardiovascular changes
- Ongoing mood and sexual health changes
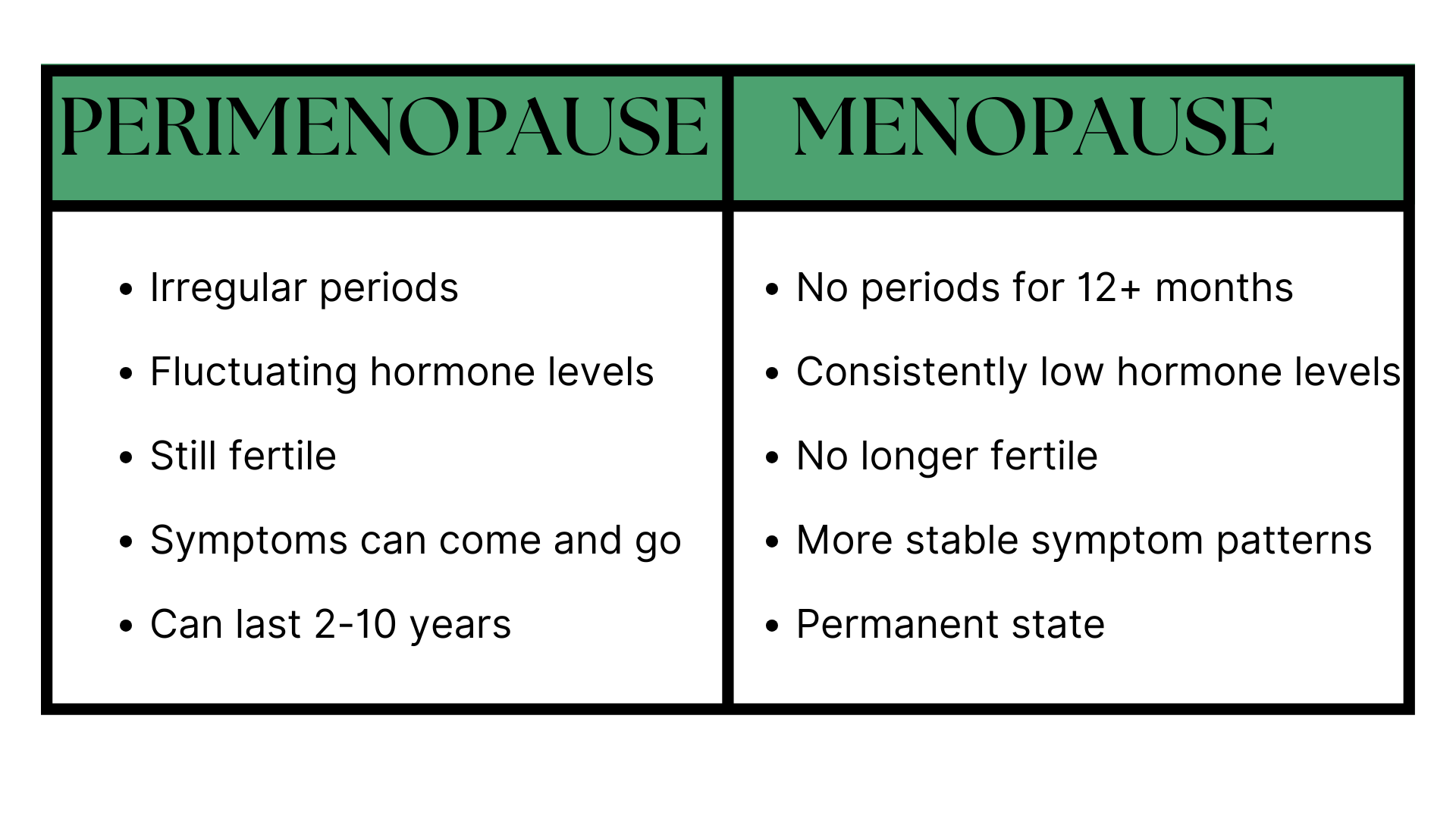
Key Differences: Perimenopause vs. Menopause
When Should You Seek Help?
During Perimenopause:
Don’t wait to get help if you experience:
- Irregular bleeding patterns
- Severe mood changes
- Hot flashes that disrupt your life
- Sleep issues affecting your daily function
During Menopause:
Seek immediate medical attention for:
- Any bleeding (this is never normal in menopause)
- Severe persistent symptoms
- New health concerns
The Functional Medicine Difference
In my practice, I take a unique approach to these transitions. While traditional medicine often focuses solely on symptom management, functional medicine looks at the whole picture. We recognize that both perimenopause and menopause symptoms are highly modifiable through lifestyle interventions and hormone balancing.
Every woman’s journey is different, which is why I believe in personalized treatment strategies backed by comprehensive testing and ongoing monitoring. Through this integrated approach, we can effectively manage symptoms while supporting your overall health.
Ready to Take Control of Your Menopause Journey?
Understanding the difference between perimenopause and menopause is just the beginning. If you’re ready to dive deeper and gain the knowledge you need to navigate this transition with confidence, I invite you to learn more in our new comprehensive online course, The Menopause Mentor.
Drawing from my experience treating hundreds of women, I’ve created a program that combines the best of both functional and traditional medicine.
You’ll get:
- Evidence-based strategies that work
- Practical solutions you can implement immediately
- A comprehensive approach to symptom management
- Long-term health optimization techniques
Don’t wait until your symptoms become unbearable. Understanding and addressing these changes early can make a significant difference in your journey through these natural life transitions.
Dr. Miiko Rowley is a board-certified physician in both Family Medicine and Functional Medicine, specializing in women’s health and hormone optimization. She has successfully treated hundreds of women through perimenopause and menopause using an integrated approach that combines traditional medical expertise with functional medicine principles.